|
Sumaiya Sayeed '20
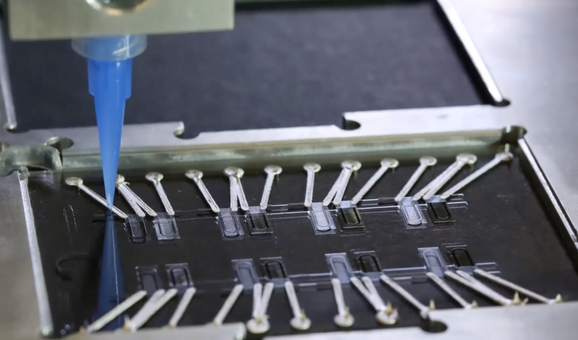
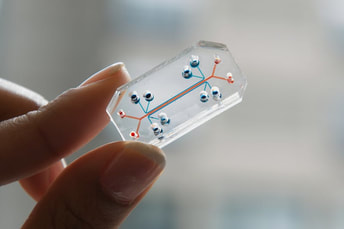 The lung on chip model, developed at the Wyss Institute, is revolutionary in the tests it allows scientists to perform. The lung on chip model, developed at the Wyss Institute, is revolutionary in the tests it allows scientists to perform. The great applications of biomedical science do not just include the ones that can directly be translated as an implant or remedy for a patient but also those that further the scope of scientific research itself. That is exactly what the heart-on-a-chip does; a small rectangular piece of plastic embedded with microfilaments, electrical connections, nutrient circulation, and mechanical simulators, this device is a large step forward in understanding the way the tissues in the heart function[1]. The organ-on-chip concept was first established at Cornell University in 1990 by Michael Shuler, who believed that growing cells in compartments interconnected with channels carrying essential nutrients would provide a better platform for in vitro studies than utilizing samples of animal tissue or culturing cells in plates. He was right; the ability to grow multiple types of cells with dynamic properties – fluid movement, membrane transport, cell interaction – would provide more functional data than would cell cultures, and having a small controlled system that can be created in the lab would bypass the need for freshly obtained animal tissues. Since 1990, the organ-on-chips have exponentially become more complex. While Shuler’s organ-on-chip consisted of cells placed in silicon wafers connected through channels, the lung-on-chip developed in 2010 includes channels for air and flowing liquid lined with pulmonary and arterial epithelial cells[2]. This model also includes the immune cells that respond to environmental factors and a vacuum chamber to mimic the movement of breathing. Having these models allows for a variety of tests to be performed – immune response, scarring, inhaled drug absorption/smoking effects (lung), and chemical response. The last one, especially, will be particularly useful for two reasons: liver toxicity, a common reason that drugs are rescinded, can be avoided if studies on livers-on-chips are done ahead of time. The second reason has an application in biodefense and epidemiology: by attacking organs-on-chips with toxins used in radiological or chemical warfare or with diseases, scientists can observe gene expression and the mechanism by which cells respond to determine new drug targets[3]. When it comes to the heart-on-chip model, significant breakthroughs are made in addressing limitations of prior models by including imitation of contractile motion, electrophysiological networks, and a greater variety of cells. What makes the heart-on-chip a significant breakthrough is the real-time data collection, drawing back to the goal of the organ-on-chip in the first place: a platform for in vitro studies. Instead of having to visually track changes in the system at certain time points, researchers can now acquire data non-invasively via electronic changes involved muscular contractions. The power of the organ-on-a-chip is great with its great simulating properties with the convenience of a small, ready-made device.
_________________ [1] Lind, Johan U. et al. Instrumented cardiac microphysiological devices via multimaterial three-dimensional printing. Nature Materials [online]. 2016 [cited 2017 Oct 4]; 16 303-308. Available from: National Center for Biotechnology Information. [2] Baker, Monya. A Living System on a Chip. Nature [online]. 2011; 471. [3] Reardon, Sara. Scientists seek ‘Homo chippiens’. Nature. 2015; 518.
0 Comments
Leave a Reply. |