|
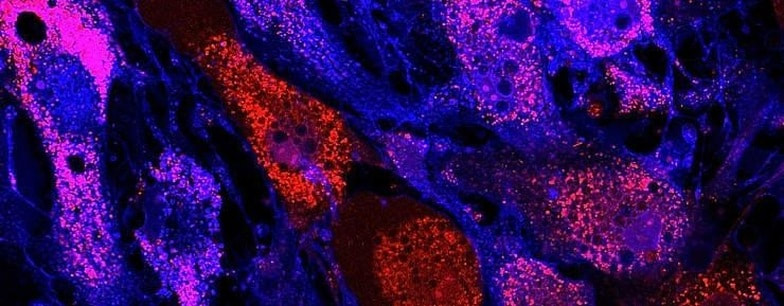
Written by Hailey Chen ‘24 Edited by Jasmine Shum ‘24 The skin is our first line of defense against external forces and infection. Comprised of 2 principal layers (the tough external epidermis and the inner dermis), it serves 3 primary purposes: protecting the body by keeping pathogens out and fluids in, regulating body temperature by controlling blood vessel dilation, and utilizing nerve pathway connections to communicate environmental stimuli to the brain. [1] It is this communication pathway that allows the body to adapt to environments through responses in the skin and surrounding tissues in order to maintain homeostasis. To varying degrees, a severe burn injury can compromise all three of these skin functions. These types of injuries can be defined as injuries in which soft-tissue damage occurs as a result of thermal heat, frictional heat, toxic chemicals, electricity, or nuclear radiation. 486,000 burn injuries each year are severe enough to warrant medical treatment in the United States [2], and these disproportionately affect people of lower socio-economic status, the very young, and the very old [3]. This isn’t just an issue locally; burns are a global public health problem, accounting for an estimated 180,000 deaths annually [3]. And while burn injuries are generally non-fatal, physical recovery is often an extremely lengthy and difficult process; burns are consistently considered to be among the most painful injuries a person can endure, and the subsequent wound care required to treat it is often even more painful than the initial trauma. [4] In addition to the immediate tissue loss after a burn injury, the injury deepens with time as the excessive inflammatory reaction progresses. Furthermore, a greater total body surface area burned correlates to a higher release of inflammatory molecules, which is associated with a higher risk of developing sepsis (a potentially fatal bacterial infection) and multi-organ failure. Prompt wound closure after a burn has been closely linked to survival, reduced complications such as infection, and hypertrophic scarring. [5, 6, 7] Consequently, a major clinical priority in the treatment of burns is rapid wound healing and mitigation of inflammatory components. To do so, the traditional method of treatment aims to close the wound by grafting the very top layers of skin from another part of the body and placing it on the injury site. Partial or full thickness burns penetrate through the epidermis, which is unfortunately the only part of the skin that can be grafted. Due to this, grafted skin is significantly mechanically inferior to healthy skin, as grafted skin has deficits in sensory skills such as touch reactivity or temperature regulation. [5, 7] Additionally, grafting technically creates another injury (usually one that spans a large surface area), though donor site injuries are controlled and often deemed to be a necessary sacrifice to maximize patient well-being and safety. Transplanted tissue also runs the risk of being rejected by the recipient site. [6, 7] Mesenchymal stem cells are being toted by scientists as a possible solution to all of these issues. The term “mesenchymal stem cell” (abbreviated as MSC) refers to cells isolated from the stroma, the connective tissue that surrounds other tissues and organs. (Cells by this name are sometimes called “stromal cells” by many scientists.) The first MSCs were discovered in the bone marrow and were shown to be capable of making bone, cartilage, muscle, neural, skin, corneal, and fat cells. [6] The field of regenerative medicine has made significant progress since the discovery of MSCs in the 1970’s; more recently, research on MSC properties has led to a renewed interest in using MSCs for cell-based therapy to facilitate cutaneous wound healing using intravenous transplantation for burn survivors. MSCs are of special interest in burn wounds (as cells can be effective on different wound beds) because they show potential in accelerating wound healing, improving skin regeneration, and minimizing scarring. [8] When first introduced, MSCs stimulate the development of new blood vessels (known as angiogenesis) and then differentiate into multilayered epidermal-like structures that aid in wound closure. They are immunoprivileged, meaning that they have the ability to avoid a negative response (such as inflammation) from a person’s immune system, which greatly reduces the risk of transplant rejection. Unlike grafted skin, MSCs are able to generate hair follicles, resulting in restored protection, regulation of body temperature, and facilitation of the evaporation of perspiration. They also aid in collagen deposition and tissue formation while reducing the risk of infection. [5, 7, 8] As this is still a relatively new field of research, most of the recent significant clinical developments in MSC use in regenerative dermal medicine have been conducted in animal trials, primarily in rats and mice. Recent studies indicate that within as soon as 7 days following an MSC injection, reduced inflammation (due to the suppression of pro-inflammatory factors) could be observed in experimental groups. [8] MSCs were shown to accumulate at the injury site, higher collagen concentrations were reported, and angiogenesis increased as well: neovascularization (the natural formation of new blood vessels) in experimental groups was markedly higher, with fine branches and networks of blood vessels observable by the naked eye. [9] The consensus was reached that wound healing was significantly accelerated in MSC animal therapy groups. [8, 9, 10, 11] The small quantity of cadaveric and live human subject trials involving MSCs have also proven to be fruitful. [12] Most reported trials describe patients with burns comprising less than a total body surface area (TBSA) of 80%; approximately 70% of those studied were partial and deep-partial thickness, not full-thickness burns. [4] In these cases, injury sites were observed to undergo rapid regeneration of epithelial skin in the epidermis without the long-term consequences of hypertrophic scar formation, which inhibit mobility and have negative psychological effects, thus demonstrating the potential of MSCs even in the acute phase of burn care. When MSC efficacy was tested in a severely injured patient with a large surface area (70% TBSA) burn, mostly full-thickness, as well as an inhalation injury with a resultant mortality risk of 80%, the patient recovered without adverse treatment complications (including keloids or hypertrophic formations) during a 6-year follow-up period. [6] These trends were mirrored in other patients with severe burn injuries whose wounds did not heal with over 18 months of conventional burn care. [7] The studies also noted the strong anti-infective properties of such treatment plans. As such, the therapeutic use of transplanted MSCs for large non-healing burn wounds was deemed safe and effective and has notable treatment potential. The progress in critical and intensive care burn management in the 21st century has significantly reduced mortality in patients with critical burn injuries. This progress has moved the focus of burns care from simple survival to the quality of life after the burn trauma. With the development of regenerative technologies, MSCs have emerged as a promising and attractive strategy to enhance tissue regeneration, homeostasis, and wound closure. While MSCs may not provide a cure, they can help the body heal and mitigate symptoms for an extended period of time, thus increasing patient quality of life. Works Cited: [1] American Academy of Orthopaedic Surgeons. Emergency Care and Transportation of the Sick and Injured. 11th ed. Pollack AN, Edgerly D, McKenna KD, Vitberg DA, editors. Sudbury, MA: Jones and Bartlett Learning; 2017. [2] Burn Incidence and Treatment in the United States: 2016 [Internet]. Burn Incidence Fact Sheet. American Burn Association; 2017[Cited 2020 October 18]. Available from: https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/ [3] Burns Fact Sheet [Internet]. Newsroom Fact Sheets. World Health Organization; [Cited 2020 October 18]. Available from: https://www.who.int/news-room/fact-sheets/detail/burns [4] Francis E, Kearney L, Clover J. The effects of stem cells on burn wounds: a review. International Journal of Burns and Trauma [Internet]. 2019 Feb 28 [Cited 2020 October 18]; 9(1), 1–12. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6420705/#:~:text=Mesenchymal%20stem%20cells%20were%20shown,performed%20using%20adenovirus%20as%20vector. [5] Jeschke MG, Rehou S, Mccann MR, Shahrokhi S. Allogeneic mesenchymal stem cells for treatment of severe burn injury. Stem Cell Research & Therapy [Internet]. 2019 Nov 21 [Cited 2020 Oct 18]; 10(1). Available from: https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1465-9 [6] Maranda EL, Rodriguez-Menocal L, Badiavas EV. Role of Mesenchymal Stem Cells in Dermal Repair in Burns and Diabetic Wounds. Current Stem Cell Research & Therapy [Internet]. 2017 [Cited 2020 Oct 18]; 12(1), 61–70. Available from: https://www.researchgate.net/publication/305348099_Role_of_Mesenchymal_Stem_Cells_in_Dermal_Repair_in_Burns_and_Diabetic_Wounds [7] Rangatchew F, Vester-Glowinski P, Rasmussen BS, Haastrup E, Munthe-Fog L, Talman M-L, et al. Mesenchymal stem cell therapy of acute thermal burns: A systematic review of the effect on inflammation and wound healing. Burns [Internet]. 2020 Sept [Cited 2020 Oct 18]; 46(6), 1–27. Available from: https://www.sciencedirect.com/science/article/pii/S0305417920303053 [8] Liu J-S, Du J, Cheng X, Zhang X-Z, Li Y, Chen X-L. Exosomal miR-451 from human umbilical cord mesenchymal stem cells attenuates burn-induced acute lung injury. Journal of the Chinese Medical Association [Internet]. 2019 Dec [Cited 2020 Oct 18]; 82(12), 895–901. Available from: https://journals.lww.com/jcma/Fulltext/2019/12000/Exosomal_miR_451_from_human_umbilical_cord.4.aspx [9] Li X, Wei Z, Zhang W, Lv H, Li J, Wu L, et al. Anti-Inflammatory Effects of Magnetically Targeted Mesenchymal Stem Cells on Laser-Induced Skin Injuries in Rats [Corrigendum] . International Journal of Nanomedicine [Internet]. 2020 Oct [Cited 2020 Oct 18]; 15(15), 5645–59. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428346/ [10] Xue L, Xu Y-B, Xie J-L, Tang J-M, Shu B, Chen L, et al. Effects of human bone marrow mesenchymal stem cells on burn injury healing in a mouse model. International Journal of Clinical & Experimental Pathology [Internet]. 2013 Jul 1 [Cited 2020 Oct 18]; 6(7), 1327–36. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3693197/ [11] Liu L, Yu Y, Hou Y, Chai J, Duan H, Chu W, et al. Human Umbilical Cord Mesenchymal Stem Cells Transplantation Promotes Cutaneous Wound Healing of Severe Burned Rats. PLOS ONE [Internet]. 2014 Feb 20 [Cited 2020 Oct 18]; 9(2), 1–8. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0088348 [12] Mansilla E, Marín GH, Berges M, Scafatti S, Rivas J, Núñez A, et al. Cadaveric bone marrow mesenchymal stem cells: first experience treating a patient with large severe burns. Burns & Trauma [Internet]. 2015 Sep 18 [Cited 2020 Oct 18]; 3. Available from: https://academic.oup.com/burnstrauma/article/doi/10.1186/s41038-015-0018-4/5670653
1 Comment
6/29/2021 05:24:29 am
This is very informative! Effective treatments for some types of hair loss are available, from nonmedical solutions to medications and surgery to promote hair growth and slow hair loss. It same as Haarlem Oil and Haarlem Oil for Human (https://genuine-haarlem-oil.com/shop/) made by French people in France very effective products also good for fighting against viruses. I love the journey of my research from this website. Hope you do more blog post here about health. Thank you and God bless
Reply
Leave a Reply. |