|
by Dahee Seo '17 We all know someone with diabetes. The Centers for Disease Control and Prevention estimated that 29 million people in the United States or 9.3% of the population had diabetes in 2014. Each diabetic has to prick his or her finger everyday, drawing out blood to avoid cardiovascular disease, stroke, or kidney failure. Why? Because patients with diabetes lack the ability to control their blood glucose level and must monitor it manually. Otherwise, their blood glucose level can shoot up and cause various side effects or drop so low that patients fall unconscious.
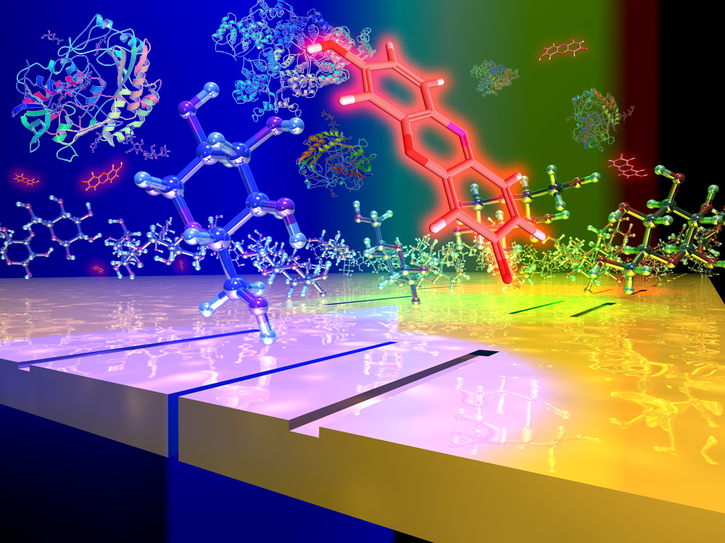
However, this discomfort may soon end for diabetics. Last year, researchers from Brown developed a new biochip sensor that can measure concentrations of glucose within artificial saliva, which consists of water, salts, and select enzymes. The new chip makes use of dye chemistry combined with plasmonic interferometry, a method of detecting the concentration of a chemical compound by using light. The biochip is a one-inch-square piece of quartz covered in a layer of silver that is engraved with thousands of nanoscale interferometers. Each interferometer consists of one slit and two grooves. When light shines through a liquid placed on one of these interferometers, some of the photons (light particles) are captured within the slit, while other photons are scattered by the grooves and interact with electrons on the silver's surface. Photons that interacted with the surface electrons move across the sensor's surface and meet photons trapped in the slit. Interference then occurs.The amount of interference directly correlates with the concentration of the liquid. By measuring the light intensity coming through each slit, the sensor is thus able to determine the liquid’s concentration. Previously, plasmonic interferometry could not be used to measure the glucose level in artificial saliva because solutes other than glucose interfered with the biochip’s response. To overcome this problem, on the biochip,researchers added channels with two enzymes: glucose oxidase and horseradish peroxidase. Glucose oxidase turns glucose into hydrogen peroxide while horseradish peroxidase turns hydrogen peroxide into resorufin. The resorufin molecule absorbs and emits red light, coloring the liquid.
When the nanoscale interferometers were tuned to detect the resorufin molecules (and thus the presence of glucose) in lab tests, the combination of the plasmonic interferometry and dye chemistry methods was sensitive enough to detect miniscule differences in glucose concentrations in the artificial saliva. The next step is to test the biochips on actual human saliva. This new technology will only become more important in the future because the number of people with diabetes is rapidly increasing. The Centers for Disease Control and Prevention predicted that if this trend continues, as many as 1 in 3 U.S. adults could have diabetes by 2050. The development of a small saliva-analyzing device would ultimately enable people with diabetes to test their sugar levels without drawing blood and causing pain. For most patients, this device would merely save them from a little discomfort. However, a saliva-analyzing device would also be hugely beneficial for diabetic children and their families Such a device would save parents from the difficult task of regularly pricking fingers of children who cry, get angry, and resist stubbornly.
0 Comments
Leave a Reply. |