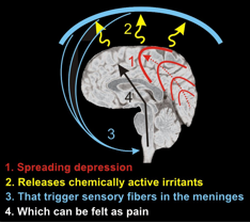
 The spreading depression theory The spreading depression theory Migraines begin to recur during adolescence, with women reporting more migraines than men. The symptoms of both migraine and sinus headache include facial pressure and pain. Because they share these symptoms, migraine is often misdiagnosed as sinus headache. Sinus headaches, unlike migraines, usually occur suddenly and without warning. Individuals suffering from headache may experience dull pain that shifts when the head is repositioned, as opposed to being constrained to one side of the head (as is the case with migraine). On the other hand, migraines may include myriad symptoms, such as unilateral throbbing pain, nausea, dizziness or chills, sensitivity to visual and auditory stimuli, and feelings of anxiety. In addition, one study showed approximately 19.7% of individuals experience an aura, during which they sense an impending migraine. Auras are characterized by sensitivity to visual stimuli, the appearance of blind spots in the visual field, as well as the distorted perception of the shape and size of objects. Migraine sufferers may also experience numbness or tingling in the extremities, sensitivity to strange smells, and weakness on one side of the body. Unlike regular headaches, migraines result from changes in cranial blood vessels. The constriction of these vessels may be responsible for early signs such as auras, whereas dilation results in the pain experienced by migraine sufferers. The trigeminovascular system consists of the neurons in the trigeminal nerve that innervate cerebral blood vessels. Although the pathology of migraine is still unclear, changes in the trigeminovascular system have long been proposed as the cause behind the pain. In the 1950s, Harold Wolff and his colleagues concluded that vasoconstriction and the resulting resistance to blood flow occur before the onset of migraine. As a migraine develops, there is vasodilation, hyperanemia, and reduced resistance to blood flow in the affected vascular bed. Their discovery propelled the drug industry’s focus on creating pharmaceuticals, such as ergotamine tartrate, that would reverse the vasodilation of the extracranial vascular system. These early studies were challenged by the fact that reversing vasodilation didn’t always alleviate migraine. This is because during the course of a migraine, many people develop cutaneous allodynia, which means that they become more sensitive to pain. Just wearing glasses or earrings can be painful. After the onset of cutaneous allodynia, vasoconstrictors such as triptans are ineffective. Due to a lack of understanding of the compounded involvement of cutaneous allodynia, migraine drug research slowed. In addition, there is a great divide in the scientific community studying chronic pain regarding which vessels are involved in migraine. Although most evidence points to extracranial arteries as the major source of migraine pain, many scientists remain convinced that the vascular pain results from intracranial vessels alone. Such disparate opinions and a lack of a unified view on the cause behind vascular pain also greatly slows the research being done on potential migraine therapies. One of the more widely researched ideas is that a phenomenon known as “spreading depression” may be one of the factors contributing to migraine. Spreading depression was first illustrated by applying a weak mechanical stimulus to the cerebral cortex of a rabbit. Briefly after the application of the stimulus, there was a decrease in spontaneous electrical activity in the affected region. The depression then spread in different directions, affecting nearby areas. Within five to ten minutes after stimulation, the spontaneous electrical activity within the stimulated region was recovered by the time the depression reached the more distant brain regions. This discovery was significant because many symptoms such as scintillating scotomas (flickering light around the center of the visual field) – which are the most common type of visual aura – and nausea may be a result of this spreading depression. The causes of migraine are very likely genetic, since migraine tends to run in families. In 2010, a group of researchers discovered a mutation in the TRESK gene, which codes for a potassium ion channel. Since potassium channels are essential for keeping a neuron at rest, mutations of these channels may result in overactive neurons that fire at lower levels of pain. Although we are still far from understanding the pathogenesis of migraine pain, directing research to explore the changes in extracranial arteries (rather than intracranial arteries), as well as performing further studies to identify more genes that play a role in migraine will edge us closer to finding a treatment for migraine pain. Despite the staggering statistic of 28 million Americans suffering from migraines, there is still a stigma associated with the condition, which is further complicated by its less obvious symptoms. A greater understanding of migraine, as well as additional research, will allow its victims to be more productive in the workplace, maintain more positive personal relationships, and become more engaged in their own lives.
0 Comments
Leave a Reply. |

